
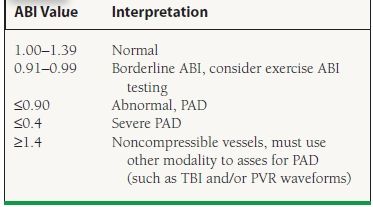

13 Little attention has been paid to the association of inflammatory markers with new-onset PAD, 14 especially in the Chinese population. 2, 3, 4, 5 There is evidence that markers of inflammation including WBC count and C-reactive protein are associated with higher mortality in patients with known atherosclerotic vascular disease 6, 7, 8 and also associated with increased risk of myocardial infarction and stroke, 9, 10, 11, 12 which shows that atherogenesis is a chronic inflammatory process and inflammation potentially plays a central role in the development and progression of systemic atherosclerosis. 1 PAD is a surrogate of systemic atherosclerosis, and patients with PAD have a significantly increased risk for premature mortality and cardiovascular events. In conclusion, elevated WBC counts independently predict the risk of new-onset PAD in a Chinese community-based population, supporting the hypothesis that systemic inflammation plays an important role in PAD development.Īccording to the Global Burden of Disease Study, although age-standardized mortality for cardiovascular and circulatory diseases has decreased by 22%, significant increases in mortality have occurred for peripheral arterial disease (PAD) from 1990 to 2013. Furthermore, we did not find significant heterogeneity among the analyzed subgroups based on sex (male or female), age (<60 or ⩾60 years old), body mass index (BMI, <25 or ⩾25 kg m −2), current smoking, current drinking, hypertension, diabetes mellitus, dyslipidemia or cardiovascular disease. The highest WBC quartile group had increased risk when compared with the lowest quartile group (OR=2.14, 95% CI: 1.09–4.22, P=0.027) in a multivariate logistic model. This relationship remained significant (OR=1.21, 95% CI: 1.08–1.36, P=0.0014) even after adjusting for other variables. WBC counts were significantly associated with PAD incidence (odds ratio (OR)=1.27, 95% confidence interval (CI): 1.14–1.41, P<0.0001) with every 1 × 10 9 l −1 increase in WBC count. The mean (±s.d.) baseline WBC count was 6.11☑.54 × 10 9 l −1, the mean (±s.d.) ABI was 1.11☐.08 at baseline and the incidence of PAD was 2.7% over 2.3 years. Multivariate regression models were used to evaluate the association of WBC count and new-onset PAD. The ankle brachial index (ABI) was measured, and PAD was defined as an ABI <0.9. A total of 3555 Chinese subjects without fever and PAD at baseline from an atherosclerosis cohort were included in our analysis. This longitudinal cohort study investigated whether peripheral WBC counts could predict peripheral arterial disease (PAD) incidence after a 2.3-year follow-up in a Chinese community-based population without PAD at baseline.


 0 kommentar(er)
0 kommentar(er)
